 |
|
#91
|
||||
|
||||
|
Re: Sexual Health News
HIV 'fingerprint' tool could greatly assist vaccine development
http://www.medicalnewstoday.com/articles/316642.php Scientists hope that their new method of "fingerprinting" the shields of sugar molecules that HIV surrounds itself with to evade the immune system will improve and speed up the development of effective vaccines. The researchers - from The Scripps Research Institute (TSRI) in La Jolla, CA - report how they developed and tested their HIV fingerprinting tool in the journal Nature Communications. According to the World Health Organization (WHO), HIV remains a persistent major problem for global public health. To date, the virus has killed more than 35 million people. Once it enters a person's body, HIV weakens the immune system. The virus impairs and destroys immune cells - especially infection-fighting CD4 cells, or T cells. As a result, the person becomes increasingly susceptible to a wide range of infections and diseases, including some types of cancer. There is currently no effective cure for HIV, but it can be controlled with antiretroviral therapy (ART). If properly administered and followed, ART can make a dramatic difference to the lives of infected people and their communities. It can keep them healthy and lower their chances of infecting others. Challenge for HIV vaccine developers AIDS is the most advanced stage of HIV infection - it can take 2 to 15 years to reach, depending on the individual. However, if HIV is diagnosed early and the disease is treated before it is too advanced, an infected person can expect to live a healthy, long, and productive life. Estimates from the Centers for Disease Control and Prevention (CDC) suggest that 1.2 million people in the United States were living with HIV at the end of 2013, including around 1 in 8 who did not know that they were infected. Great progress has been made in preventing and treating HIV, but there is still much to do, including the search for a vaccine. Two of the major challenges facing HIV vaccine developers are that the virus is good at hiding from the immune system, and that it keeps changing. The idea of a vaccine is to stimulate the immune system to produce new or more antibodies against a target on the infecting agent that disables it. In the case of HIV, vaccine developers suggest that a good target is the glycoprotein envelope that surrounds the virus and contains the machinery that the virus uses to enter host cells. However, one of the reasons that HIV is so resilient is that it covers its glycoprotein envelope with a shield made of sugar molecules called glycans. The shield helps the virus to hide from the immune system and stops antibodies from attacking the glycoprotein envelope. Spotting 'holes' in the glycan shield Tools that help vaccine developers to deal with the glycan shields are enormously helpful. The new study offers such a tool in the form of a method that analyzes patterns of glycans on the glycoprotein. It allows scientists to quickly "fingerprint" the virus and tell if their vaccine development is on the right track. An important requirement is the ability to distinguish between high-mannose glycans and complex-type glycans on the glycoprotein envelope. Previous studies have reached this point. However, the new study goes further in that it also identifies glycoprotein sites that have no glycans. In fact, the team found that there are fewer such "holes" in the shield than previously thought. Finding sites with no glycans is important because vaccine developers can then devise a way to teach the immune system to recognize where the holes in the glycan shield are and produce broadly neutralizing antibodies that attack the underlying envelope. The new tool is also fast; the team developed algorithms that quickly analyze the results much faster than the manual methods that they were using before. Analysis speed is important in this field as developers are always in a race against time searching for vaccine candidates to fight a virus that evolves rapidly. Next step: Work with natural forms of HIV In their study, the researchers used an HIV-like vaccine candidate. They now plan to use the new tool to analyze glycan composition and glycan-free sites on natural forms of HIV. If the fingerprints match up with what they have, then they will know that they are on the right track. Quote:
The new study went some way toward showing this, in that the team also tested the method on an influenza virus protein. |
|
#92
|
||||
|
||||
|
Re: Sexual Health News
Vaginal itching: Common causes, symptoms, and treatments
http://www.medicalnewstoday.com/articles/316595.php Vaginal itching is an uncomfortable, yet common occurrence. There are a number of causes, and most require medical treatment. This article provides an overview of common causes of vaginal itching, along with links to more detailed articles. Contents of this article: Yeast infections Bacterial vaginosis (BV) Sexually transmitted diseases (STDs) Irritation or allergy Yeast infections Most women will experience a vaginal yeast infection during their lifetime. Though these aren't usually serious, yeast infection symptoms can be bothersome. Normally, a balance of healthful bacteria and yeast live in the vagina. The bacteria keep yeast in check, preventing overgrowth. When the vagina's bacteria do not properly control the yeast balance, yeast overgrowth can occur. Symptoms of yeast overgrowth can include: itching burning odorless white or clear discharge irritation Yeast infections usually occur when something upsets the vagina's bacteria balance. Common causes include: douching hormone changes, such as during pregnancy, or from using hormonal birth control use of antibiotics Some health conditions may also make a woman more likely to get a yeast infection. A weakened immune system or uncontrolled diabetes may increase the risk. Bacterial vaginosis (BV) This common bacterial infection, also known as BV, often affects women of childbearing age. BV occurs when the normal, healthful bacteria in the vagina become unbalanced. Many women who get BV have no symptoms. However, it can cause a watery vaginal discharge with an unpleasant odor, as well as burning and itching around the vaginal area. The cause of BV isn't always known. But, in many cases, BV is caused by one of the following: douching, which may upset the vagina's natural bacteria bathing with antiseptic or antibacterial products having a new sex partner or multiple sex partners using strongly scented products in the vaginal area harsh clothing detergents smoking Many women may get BV and not know it, since it often causes no symptoms. However, it can be potentially dangerous to a pregnant woman and her fetus. A pregnant woman should discuss any vaginal itching, burning, or discharge with her doctor and get tested for BV when needed. A BV test involves taking a sample of fluid from the vagina and sending it to a lab for analysis. If the test is positive, a pregnant woman will likely undergo treatment with antibiotics. Because BV is a result of an imbalance of bacteria, replacing the body's "friendly" bacteria may be helpful in some women. A 2014 review found that certain probiotics, when taken by mouth, might help prevent or treat BV. The probiotics studied were Lactobacillus acidophilus, Lactobacillus rhamnosus GR-1, and Lactobacillus fermentum RC-14. Sexually transmitted diseases (STDs) STDs, also known as sexually transmitted infections (STIs), can occur as a result of having sexual contact with an infected person. The Centers for Disease Control and Prevention (CDC) say that STDs are at an unprecedented high in the United States, with millions of cases reported each year. People can reduce the risk of getting an STD by: abstaining from sex using a condom correctly each time having fewer sex partners getting tested for STDs before having sex getting treatment when needed getting the HPV (human papillomavirus) vaccine Many STDs can cause vaginal itching, among other symptoms. It's important to have STDs treated, as some may cause long-term problems such as pelvic inflammatory disease, infertility, and pregnancy complications. A woman can also pass certain STDs to her baby during childbirth.   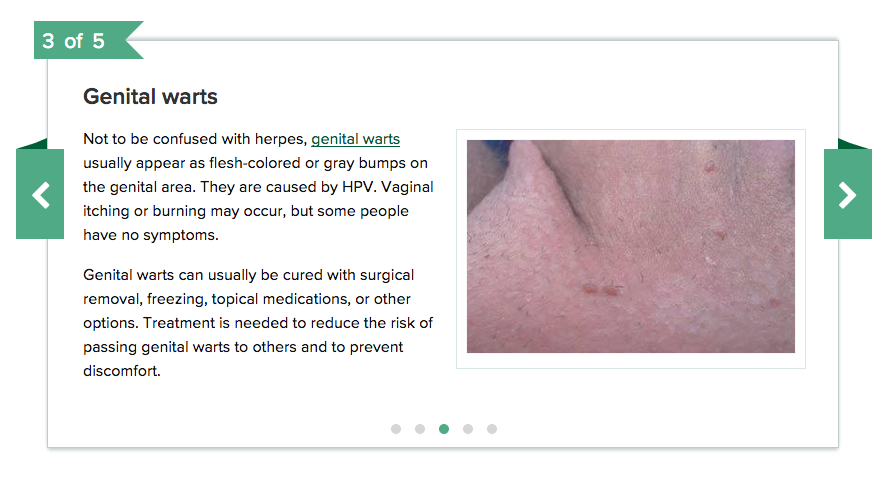 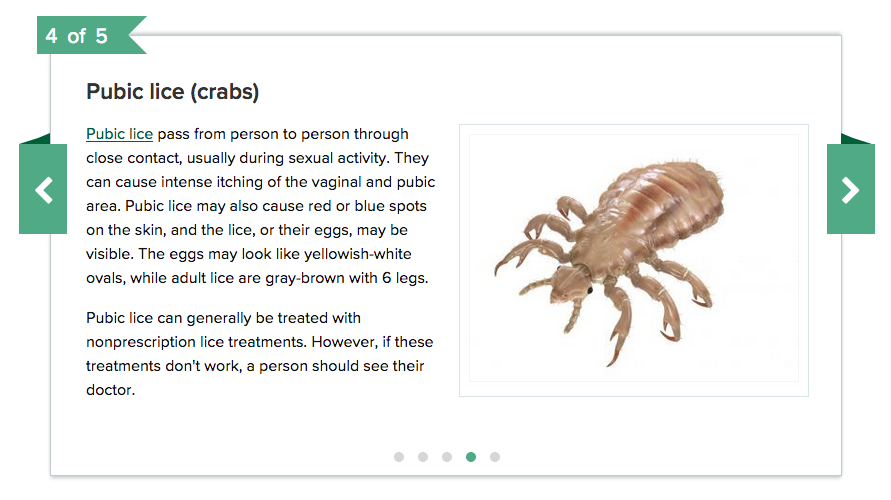  Irritation or allergy In some cases, minor vaginal itching may result from using scented laundry detergent or feminine products such as pads, tampons, or feminine deodorants. The itching will usually go away after a woman stops using these products. To avoid this issue, women may choose to use products labeled "fragrance free" or "unscented." Douching is also not recommended, as it may lead to vaginal irritation, BV, and yeast infections. Some women may have an allergic reaction to latex condoms, which may result in vaginal itching or irritation. People who suspect they might be allergic to latex condoms should ask their doctor about alternatives. Although vaginal itching can be embarrassing or bothersome, most cases of it can be treated by consulting a doctor. To help avoid possible long-term health problems, it's best to push aside any embarrassment and determine the cause of the itching, so proper treatment can be provided.
__________________
You are my forum, my only forum, you make me happy, when skies are grey... Sex health related questions click here. WOMEN'S CHARTER click here Sg law on sex related matters click here Last edited by Big Sexy; 05-06-2017 at 10:28 AM. |
|
#93
|
||||
|
||||
|
Re: Sexual Health News
NIH scientists advance understanding of herpesvirus infection
http://www.medicalnewstoday.com/releases/316950.php Herpes simplex virus (HSV) infections last a lifetime. Once a person has been infected, the virus can remain dormant (latent) for years before periodically reactivating to cause recurrent disease. This poorly understood cycle has frustrated scientists for years. Now, National Institutes of Health scientists have identified a set of protein complexes that are recruited to viral genes and stimulate both initial infection and reactivation from latency. Environmental stresses known to regulate these proteins also induce reactivation. Globally, the World Health Organization estimates that 500 million people are infected with HSV-2 while two-thirds of the population are infected with HSV-1. These viruses cause human diseases ranging from oral cold sores to genital lesions to serious eye conditions that can lead to blindness. In infants, HSV can cause neurological and developmental problems. People infected with HSV also have an enhanced risk of acquiring or transmitting human immunodeficiency virus (HIV). Scientists at NIH's National Institute of Allergy and Infectious Diseases previously made progress toward understanding the role of cellular protein HCF-1 in initiating HSV infection and reactivation. HCF-1 and associated proteins are recruited to the viral genome to enable the virus to replicate and spread. This previous work identified targets for the development of therapeutics to suppress infection and reactivation. Their latest work, with collaborators from Princeton University, Princeton, New Jersey, identifies new HCF-1 protein complexes that play additional roles in initiating viral infection and reactivation. The scientists found they could reactivate latent HSV in a mouse model using compounds that turn on components of these HCF-1 protein complexes. Interestingly, some of these HCF-1-associated proteins also are involved in HIV reactivation from latency. The researchers are continuing to investigate the protein complexes involved in promoting HSV gene expression, infection, and reactivation from latency. Identifying these complexes and understanding the mechanisms by which they function can potentially reveal additional targets for the development of new therapeutics. Article: Transcriptional Elongation of HSV Immediate Early Genes by the Super Elongation Complex Drives Lytic Infection and Reactivation from Latency, R. Alfonso-Dunn et al., Cell Host & Microbe, doi: 10.1016/j.chom.2017.03.007, published 12 April 2017. Thank you for supporting Medical News Today |
|
#94
|
||||
|
||||
|
Re: Sexual Health News
Gonorrhea bacterium manipulates an anti-infection mechanism in the female reproductive tract
http://www.medicalnewstoday.com/releases/316971.php The bacterium that causes gonorrhea infects the female reproductive tract by breaking connections between cells in the tract's protective lining, according to new research published in PLOS Pathogens. Gonorrhea is a widespread sexually transmitted disease caused when Neisseria gonorrhoeae bacteria infect the normally protective inner lining of human genital tissues. In women, the opening of the uterus, known as the endocervix, serves as a primary infection site for N. gonorrhoeae. However, the strategy used by N. gonorrhoeae to penetrate the lining of the endocervix has been unclear. To investigate this mechanism, Liang-Chun Wang of the University of Maryland, College Park, and colleagues needed to develop an alternative to the mouse models normally used to study gonorrhea, since they have been inadequate for this purpose. The team developed a new model using tissue samples obtained from the human endocervix. The researchers infected the endocervix tissue, as well as lab-grown cells of the same type as those that line the endocervix, with N. gonorrhoeae. They then employed a variety of molecular and imaging techniques to examine the infection mechanism. The results demonstrate that N. gonorrhoeae penetrates the endocervix lining by interfering with a normally protective process. Usually, infected cells in the lining can be shed and disposed of without breaking the tight connections between cells that keep the lining uncompromised. N. gonorrhoeae appears to be able to break these connections and induce cell shedding, opening paths for penetration without reducing its ability to adhere to and invade the cells of the lining. The scientists showed that N. gonorrhoeae causes disruption of cellular connections and cell shedding by promoting activation and accumulation of a human protein known as non-muscle myosin II. Depending on the particular genes being expressed by N. gonorrhoeae at any given time, the team found, it can either promote or inhibit this penetration mechanism. This study represents the first laboratory demonstration of the penetration of N. gonorrhoeae into the human endocervix and provides new insights into gonorrhea infection. Article: Neisseria gonorrhoeae infects the human endocervix by activating non-muscle myosin II-mediated epithelial exfoliation, Wang L-C, Yu Q, Edwards V, Lin B, Qiu J, Turner JR, et al., PLOS Pathogens, doi:10.1371/journal.ppat.1006269, published 13 April 2017. |
|
#95
|
||||
|
||||
|
Re: Sexual Health News
Oral contraceptives reduce general well-being in healthy women
http://www.medicalnewstoday.com/releases/317005.php One of the most common combined oral contraceptive pills has a negative impact on women's quality of life but does not increase depressive symptoms. This is shown by a major randomised, placebo-controlled study conducted by researchers at Karolinska Institutet in Sweden in collaboration with the Stockholm School of Economics. The results have been published in the scientific journal Fertility and Sterility. "Despite the fact that an estimated 100 million women around the world use contraceptive pills we know surprisingly little today about the pill's effect on women's health. The scientific base is very limited as regards the contraceptive pill's effect on quality of life and depression and there is a great need for randomised studies where it is compared with placebos," says professor Angelica Lindén Hirschberg at the Department of Women's and Children's Health at Karolinska Institutet. She has led just such a study together with Niklas Zethraeus, associate professor at the Department of Learning, Informatics, Management and Ethics, Anna Dreber Almenberg from the Stockholm School of Economics, and Eva Ranehill of the University of Zürich. 340 healthy women aged between 18 and 35 were treated randomly over the course of three months with either pills with no effect (placebos) or contraceptive pills containing ethinylestradiol and levonorgestrel, the most common form of combined contraceptive pill in Sweden and many other countries. Neither the leaders of the experiment nor the subjects knew which treatment was given to which women. The women who were given contraceptive pills estimated their quality of life to be significantly lower than those who were given placebos. Both general quality of life and specific aspects like mood/well-being, self-control and energy level were affected negatively by the contraceptives. On the other hand, no significant increase in depressive symptoms was observed. Since the changes were relatively small, the results must be interpreted with a certain amount of caution, the researchers emphasise. In the case of individual women, however, the negative effect on quality of life may be of clinical importance. "This might in some cases be a contributing cause of low compliance and irregular use of contraceptive pills. This possible degradation of quality of life should be paid attention to and taken into account in conjunction with prescribing of contraceptive pills and when choosing a method of contraception," says Niklas Zethraeus. The type of combined contraceptive pill that was used in the study (etinylestradiol + levonorgestrel) is recommended in many countries as the first choice since it is considered to entail the least risk of thrombosis among the combined contraceptive pills. The findings from the study cannot be generalised to other kinds of combined contraceptive pills because they may have a different risk profile and side-effects. The study was supported by research grants from Jan Wallander and Tom Hedelius Foundation, Knut and Alice Wallenberg Foundation, Swedish Council for Working Life and Social Research, the Swiss National Science Foundation, the Swedish Research Council, Karolinska Institutet, and the regional agreement on medical training and clinical research (ALF) between Stockholm County Council and Karolinska Institutet. Article: A first choice combined oral contraceptive influences general well-being in healthy women - a double-blind, randomized, placebo-controlled trial, Niklas Zethraeus, Anna Dreber, Eva Ranehill, Liselott Blomberg, Fernand Labrie, Bo von Schoultz, Magnus Johannesson, Angelica Lindén Hirschberg, Fertility and Sterility, doi:10.1016/j.fertnstert.2017.02.120, published online 18 April 2017. |
|
#96
|
||||
|
||||
|
Re: Sexual Health News
Hi, thanks much for this great information, got a good knowledge. camping for more. praise.. praise.
__________________
Welcome to exchange points. |
|
#97
|
||||
|
||||
|
Re: Sexual Health News
Diabetes and erectile dysfunction: What is the connection?
http://www.medicalnewstoday.com/articles/317012.php Erectile dysfunction, also called impotence, is not being able to get and maintain an erection for long enough to have sexual intercourse. There are many causes of erectile dysfunction (ED) which can be physical, psychological, or both. One of the most common causes of ED is diabetes. Studies suggest that 35-75 percent of men with diabetes will go on to develop ED. They will also tend to develop ED some 10-15 years earlier than men without diabetes. Why can diabetes cause erectile dysfunction? Diabetes can cause ED because it can damage the blood supply to the penis and the nerves that control an erection. When a man becomes sexually aroused, a chemical called nitric oxide is released into his bloodstream. This nitric oxide tells the arteries and the muscles in the penis to relax, which allows more blood to flow into the penis. This gives the man an erection. Men with diabetes struggle with blood sugar level swings, especially if their condition isn't managed poorly. When their blood sugar levels get too high, less nitric oxide is produced. This can mean that there is not enough blood flowing into the penis to get or keep an erection. Low levels of nitric oxide are often found in those with diabetes. Other causes of erectile dysfunction Listed below are some other reasons for ED: obesity, high blood pressure, and high cholesterol hormonal problems such as low testosterone psychological problems including stress, anxiety, and depression nervous system problems including damage to spinal cord or brain smoking, drinking too much alcohol, and using some illegal drugs some medications such as those taken for high blood pressure and depression Pelvic injury or surgery on the prostate, bowel or bladder may cause damage to nerves connected to the penis. This nerve damage can also lead to ED. Tests and diagnosis A doctor will often perform some of the following tests to diagnose ED: Blood tests to check for a raised blood sugar level, which may indicate diabetes. Hormone tests to measure the levels of testosterone and other hormones. Nervous system tests, such as blood pressure and sweat tests, which can rule out nerve damage to the heart, blood vessels, and sweat glands. Urinalysis to test for sugar in urine, which might indicate diabetes. Physical examination to assess the genitals and nerve reflexes in the legs and penis. Patient history to help determine why someone is having problems with erections and under what circumstances. Sexual health (SHIM) questionnaire to help diagnose the presence and severity of ED. Injection of a drug into the penis to check that the blood supply to the penis is normal. Lifestyle changes Erectile dysfunction due to diabetes is much better understood now. Good control of diabetes can reduce the risk of ED. Other preventive measures such as stopping smoking and reducing alcohol intake will help lower the risk of developing ED. Other lifestyle changes that may help include: Eating a healthy diet and taking exercise: Studies suggest that men who changed their diet to one low in saturated fat and high in fiber and did moderate physical activity each week were able to improve ED without prescription drugs. Weight loss: Some studies show that even a small weight loss can improve erectile function and sexual desire in men with diabetes. Those who lost weight had increased testosterone levels and blood flow resulting in better erections. Stress reduction: ED can cause stress and tension in a relationship. Counseling can be helpful even if the origins of sexual dysfunction are physical. People with ED should try to find time for relaxation and get enough sleep every night. A new study also suggests that supplementation with amino acids called l-arginine and l-citrulline may also help to improve erectile function. These acids are known to increase the body's production of nitric oxide, which can increase blood flow to the penis. As stated previously, low levels of nitric oxide are often found in men with diabetes. Treatments Treatment of ED will depend on the cause and there is a range of good treatment options. These are the same for men with diabetes and men who have ED from other causes. Doctors can switch any prescription medications that may contribute to ED. The most common treatment is with oral tablets. These have been shown to work well in many men with diabetes, restoring sexual function. Certain drugs called PDE-5 inhibitors are used to treat ED. The four most commonly prescribed are: sildenafil (Viagra) vardenafil (Levitra) tadalafil (Cialis) avanafil (Spedra) These drugs cause an erection by increasing blood flow to the penis. They require sexual stimulation to be effective. They should be taken 30-60 minutes before sexual intercourse. There are several other forms of treatment for ED. These include: Hormone therapy: Testosterone replacement therapy is recommended for men with ED who show low levels of testosterone. Penile injection therapy: Injection of alprostadil (Caverject) directly into the penis before intercourse has been approved for men who do not respond to oral drug therapy. This hormone injection increases the blood supply to the penis to produce an erection. Vacuum pump therapy: A plastic tube connected to a pump is placed over the penis. The pump empties the air out of the tube and this causes blood to be drawn into the penis. A ring is then placed on the base of the penis to maintain the erection during intercourse. Penile prosthesis: This is only considered when all other treatment options have failed as it requires major surgery. An inflatable rod is implanted into the penis to make it erect for intercourse. Psychological support: If erectile dysfunction is caused by psychological conditions, such as anxiety or depression, the patient may benefit from counseling. A well-balanced diet, exercise, and good stress management have been shown to be equally important in treating diabetes |
|
#98
|
||||
|
||||
|
Re: Sexual Health News
Porn-induced erectile dysfunction: How does it happen?
http://www.medicalnewstoday.com/articles/317117.php Men who have erectile dysfunction are unable to get or keep an erection long enough to engage in sexual intercourse. An erection normally occurs when blood flow increases into the penis, causing it to expand and become firm. Erectile dysfunction symptoms might include: trouble getting an erection trouble keeping an erection reduced sexual desire Contents of this article: Porn and erectile dysfunction Other causes of ED Related health problems Porn and erectile dysfunction Erectile dysfunction (ED) has been increasing in sexually active men under 40. It seems as though internet porn is in some ways to blame for this rise, with studies showing a correlation between porn and ED. Now, researchers have identified pornography-induced erectile dysfunction (PIED) and pornography-induced abnormally low libido. High exposure to pornography videos can result in lower responsivity in a man and an increased need for more extreme or kinky material for him to become aroused. Due to porn overload, some men are no longer aroused in the presence of a partner. They begin to experience ED and can only become sexually excited when watching porn. The role of the brain It is necessary to understand how the brain works to be able to understand why watching excessive amounts of porn can lead to ED. Neurons are cells that receive and send messages between the body and the brain. The brain has about 100 billion neurons, which are the basic working units of the nervous system. Neurotransmitters send chemical messages between the neurons. A neurotransmitter called dopamine helps the flow of information to the front of the brain, which is linked to thought and emotion. It is also linked to reward systems. Brain cells are activated by what people see or hear. If a person receives a hug, the brain releases dopamine, which makes the person feel good. A person's response to natural rewards such as sex are largely regulated by the dopamine pathway as well. Erections are dependent on the activation of this pathway. Dopamine signaling plays a crucial role in sexual arousal and erections. Dopamine overload When a person watches porn, their brain is flooded with dopamine. Too much dopamine can cause problems. The brain is overwhelmed by the overload of chemicals, and it automatically takes away some of the dopamine receptors. Although the brain continues to release the same levels of dopamine in response to porn, eventually there are fewer receptors to receive the messages. Watching porn no longer arouses the person as much or as quickly. They then have to look at more porn or search for stronger porn to obtain the original sensation. Sexual activities that would normally give people a burst of dopamine and make them happy are no longer enough to sustain them. They constantly have to look at porn to get the sensation they need, and this can lead to ED. Many men find themselves unable to maintain an erection in the absence of porn. The internet and other avenues provide an unlimited amount of content, so some men begin to watch massive amounts of porn to maintain high levels of sexual arousal. When they try to engage with a real sexual partner, the arousal they feel does not fit their expectations and they are unable to maintain an erection. Porn-induced ED Porn is designed to capture attention. The performers often do things that would typically not translate into real life. The men watching can become conditioned to this type of sexual arousal that does not carry over into real life sexual situations. Regular sex no longer meets the person's expectations, resulting in a decline in dopamine. This can cause some men to no longer be "in the mood." Men who suffer from ED when in the presence of a partner but have no problems when watching porn are said to have PIED. Studies have shown that some men with ED who watched porn were able to obtain a regular erection once the porn was removed. However, the younger the age of the male when they begin to regularly watch porn, the greater the chance of it becoming their preference over partnered sex, and the less overall enjoyment they get. PIED can also lead to other health problems. Many men recognize that there is a problem but are unable to break the cycle. They can become embarrassed or depressed when unable to perform with their partner, which can cause them to watch porn more. Other causes of ED Male sexual arousal is a complex process that involves many different parts working together. The brain, hormones, emotions, nerves, muscle, and blood vessels all have roles. ED can be due to physical, psychological, and even emotional issues. Physical causes of ED can be due to damage to the nerves, arteries, smooth muscles, and tissues in the penis. Certain medical conditions can also lead to ED, including: high blood pressure diabetes atherosclerosis, or the buildup of fats inside the arteries heart and blood vessel disease chronic kidney disease multiple sclerosis injury to the pelvic area surgery for bladder cancer prostate cancer, radiation, and prostate surgery Psychological or emotional issues that can contribute to ED include: anxiety depression or low self-esteem fear of sexual failure guilt stress A person's overall lifestyle also can play a role in the development of ED. Smoking, drinking too much alcohol, using illegal drugs, being overweight, and a lack of physical exercise can all be causes. ED is also a side effect of some common medications. Related health problems ED can be embarrassing for some men and they do not seek medical treatment to correct the problem. PIED was only recently discovered, and so men are often believed to have some medical or mental condition that is responsible for their ED. Lower sexual satisfaction and sexual dysfunction: Studies have shown that some men have to use porn to become aroused with a partner. Others have developed negative feelings toward partnered sex. Risky behavior: For some men, porn increases their need for multiple sex partners, more alcohol, drugs, and other risky behavior. They often do not use protection and have no fear of the consequences of their actions. The relationship between porn and ED is still being understood. Research has helped to show why more younger men have been experiencing erectile problems. Porn addiction is serious and should not be taken lightly. There are treatment programs available to help men with the condition. Some men may not realize that they have an addiction and may be unsure how to get help. The good thing about this type of erectile disorder is that it is generally very treatable and reversible. |
|
#99
|
||||
|
||||
|
Re: Sexual Health News
Prostate cancer: Stages and outlook
http://www.medicalnewstoday.com/articles/317586.php Prostate cancer is a male-only disease and is the second most common male cancer in the United States, after skin cancer. In the case of prostate cancer, the American Cancer Society estimate that there will be about 161,360 new cases and about 26,730 men will die from prostate cancer in the United States in 2017. As with cancers elsewhere in the body, some aggressive prostate cancers can grow and spread rapidly, while most grow slowly. Contents of this article: Prostate cancer stages Treatment Outlook Prostate cancer overview Prostate cancer stages Doctors and people who have cancer refer to the disease in terms of stages 1, 2, 3, or 4. These stages are just part of a much more complicated system that is used to categorize cancer and how far it has spread. When looking at prostate cancer, the standard is the American Joint Committee on Cancer (AJCC) TNM system. Here, those stages are defined as T1 to T4. The T of TNM relates to the growth and location of the main tumor: T1 These tumors are found either during a procedure called a transurethral resection of the prostate (TURP), which is used to treat abnormal growth of the prostate, or during a needle biopsy. A needle biopsy is a test used to investigate a rise in prostate-specific antigen (PSA). There are three different types of T1 tumor, categorized according to how the cancer is detected: T1a: detected during TURP, cancer is present in 5 percent, or less of the tissue removed T1b: detected during TURP, cancer is present in over 5 percent of the tissue removed T1c: discovered during needle biopsy T2 These tumors are larger than T1 tumors and are divided into three types according to their size and location: T2a: present in one half or less of one side of the prostate T2b: present in more than one half of one side of the prostate T2c: present in both sides of the prostate T3 These tumors have grown outside of the prostate. T4 These tumors have grown into the tissues outside of the prostate. N shows if the cancer has spread to lymph nodes while M denotes whether or not it has spread, elsewhere in the body. This staging system also relies on two other important factors. These are the level of PSA in the blood at the time of diagnosis and the Gleason score. PSA is a protein that appears in higher levels in the bloodstream when there is a problem with the prostate. The Gleason score reflects how cancerous the cells appear and how likely that a tumor will spread. Both factors are determined either through a biopsy or surgery. Stage 1 Stage 1 prostate cancers are small and grow slowly. They are still within the prostate and are unlikely to be detected during an examination by a doctor. Both Gleason scores and PSA levels are low. They may not result in symptoms or other health problems. Stage 2 Stage 2 cancers are also inside the prostate but can be felt by a doctor as they are larger than stage 1 cancers. They have higher Gleason scores or greater PSA levels, or both than stage 1 cancers. There are two types of stage 2 prostate cancers, identified according to the size and location of the tumor: The two types are 2a and 2b. Prostate cancers that are defined as 2a can be T1 tumors with high PSA or Gleason scores, or T2a or T2b with lower PSA or Gleason scores. Prostate cancers that are identified as 2b will be T2c tumors, or T2a or T2b tumors with very high PSA or Gleason scores. Stage 3 Stage 3 cancers have grown immediately outside the prostate. They may have reached the seminal vesicles but not the bladder or rectum. The seminal vesicles are glands that secrete a fluid that helps make up the semen. Cancers that have developed to this stage are more likely to return after treatment. Stage 4 Stage 4 cancers are the most serious as they have spread more widely to other areas. These are likely to include nearby organs, such as the bladder, rectum, or nearby lymph nodes. They may have even spread to distant organs, which can include bones. While a few may be curable, most stage 4 cancers are not. With incurable cancers, the aims of treatment are to keep the cancer controlled for as long as possible and to improve the quality of life. Treatment As with any serious illness or disease, the ever-important decision about treatment needs to be made after much thought and discussion. Both the man and his doctor need to evaluate all options before making the final choice. Men may also want to consider the opinions of their family and friends. Depending on the type of prostate cancer, a man may decide not to have any treatment at first. If the prostate cancer is caught early, there are many things that a person needs to consider. These considerations include general health, age, and whether the cancer is likely to cause a problem. Even when diagnosed at a later stage, there is still a lot to consider, such as possible side effects of the various treatments. Side effects can include erectile dysfunction and loss of bladder control, although these are both treatable. Treatments can include: watchful waiting or active surveillance surgery, including removal of the prostate gland radiation therapy to kill cancer cells cryotherapy, a treatment that kills cancer cells with cold temperatures hormone therapy to reduce the effect that male hormones in the body have on cancer cells chemotherapy, involving the use of anticancer drugs vaccine treatment, which directs the immune system to attack cancer cells Outlook The good news is that many men survive prostate cancer, especially if it is diagnosed in its early stages. About 1 in every 7 men is diagnosed with prostate cancer, but most of them will survive. In fact, of every 39 men who develop prostate cancer, just one will die from the disease. There are more than 2.9 million men in the U.S. who are still alive after having been diagnosed with prostate cancer. According to the American Cancer Society, of the men diagnosed with prostate cancer: the 5-year relative survival rate is almost 100 percent the 10-year relative survival rate is 98 percent the 15-year relative survival rate is 95 percent Prostate cancer overview Cancer involves cells growing out of control. These cancer cells can take hold almost anywhere in the body and can metastasize, or spread, to other areas or organs. In prostate cancer, it is cells of the male-only prostate gland that grow out of control. The prostate is a part of the reproductive system that is located just below the bladder. It plays a vital role at the time of ejaculation, secreting a milky fluid to flow into the urethra. There are different types of prostate cancers but the most common are known as adenocarcinomas. These are derived from the cells that produce the prostate fluid before it is introduced into the semen. Other types of prostate cancers include small cell carcinomas, transitional cell carcinomas, neuroendocrine tumors, and sarcomas, but these are all rare. |
|
#100
|
||||
|
||||
|
Re: Sexual Health News
Prostate cancer surgery: Types and what to expect
http://www.medicalnewstoday.com/articles/317591.php The most common form of surgery for prostate cancer is a radical prostatectomy. This surgery is when the prostate gland is removed under general anesthesia. Radical prostatectomy is not the only form of treatment for prostate cancer, and not everyone who has the condition will have surgery. Contents of this article: Staging prostate cancer Who needs surgery? Types of prostate cancer surgery Life after surgery Staging prostate cancer Prostate cancer is the second most common form of cancer in American men, behind skin cancer. The American Cancer Society estimate that there will be around 161,360 new cases of prostate cancer in 2017, and 26,730 deaths from the disease. The prostate is a gland that sits between the penis and the pelvis and produces the white sticky liquid that is mixed with sperm to make semen. The type of treatment offered depends on how advanced the prostate cancer is. This is known as the stage of cancer. Stage 1: The cancer is smaller than one half of the prostate and is contained within the gland. This is known as localized prostate cancer. Stage 2: The cancer is larger than one half of the prostate, but is still located within the gland. This is also known as localized prostate cancer. Stage 3: The cancer has broken through the outer layer of the prostate and may have spread into the seminal vesicles, the tubes that carry semen. This is known as locally advanced prostate cancer. Stage 4: The cancer has spread to another part of the body. This may be nearby lymph nodes or organs such as the rectum or bladder, or the pelvis, bone, lungs or liver. This is known as advanced or metastatic prostate cancer. Who needs surgery? Men diagnosed with prostate cancer may be offered surgery, depending on various factors. These include their age, overall health, and the stage of the cancer. Not everyone who is diagnosed will be treated for prostate cancer, as the treatments come with side effects that can affect quality of life. Because prostate cancer grows slowly, doctors may recommend watchful waiting or active surveillance, if the condition is not causing any symptoms. Watchful waiting or active surveillance mean being monitored closely for signs that the cancer is growing. Treatment will only be offered if and when it is necessary. Types of prostate cancer surgery There are two main types of prostate cancer surgery: radical prostatectomy and transurethral resection of the prostate (TURP). Radical prostatectomy A radical prostatectomy may be offered to men with localized prostate cancer who are otherwise fit and healthy. If the cancer has spread outside of the prostate, this operation may not be suitable. During a radical prostatectomy, the whole prostate gland, and the cancer within it, are removed. The seminal vesicles are also taken out, along with the nearby lymph nodes, if there is a risk the cancer may have spread to them. The type of radical prostatectomy performed will depend on the hospital. Keyhole surgery, also called a laparoscopy or minimally invasive surgery, involves the surgeon making five or six cuts in the abdomen to remove the prostate. This is done by hand with the surgeon guided by a camera and lighted tube. In robot-assisted surgery, the surgeon uses three robotic arms controlled from a computer. During open surgery or retropubic prostatectomy, a single cut is made in the stomach. A less common form of open surgery is a perineal prostatectomy. This is when a cut is made between the testicles and the back passage. Advantages Removing the prostate can remove the cancer if it is contained within the gland. Disadvantages The prostate is involved in making semen. Removing it means that men are unable to ejaculate or to father children through sex. After surgery, men experience "dry orgasms," which is the sensation of orgasm without the ejaculation. This may feel different to the experience men are used to having. Men planning on having a radical prostatectomy can consider storing sperm for fertility treatment at a later date. Risks As with all surgery, the removal of the prostate gland carries risks. These include: bleeding injury to nearby organs such as bowel and nerves blood clots infection Side effects The most common side effects are leaking urine, known as urinary incontinence, and difficulty getting or keeping an erection, known as erectile dysfunction. After surgery, most men cannot control their bladder properly. Some may experience stress incontinence, which means leaking just a few drops of urine during exercise, coughing, or sneezing. Others may need absorbent pads or pants, though this usually improves with time. Some men have difficulty urinating after the operation, and this can happen gradually or very suddenly. Most men who have this kind of surgery suffer erectile dysfunction. Surgeons will try to save the nerves that control erections, but this is not always possible. Even if nerves are saved, many men still have difficulty with erections. It can take between a few months and 3 years for erections to return, but some men will always need help or medication. TURP A TURP operation does not cure the cancer. It helps with one of the most common symptoms of prostate cancer, which is difficulty passing urine. This happens when the enlarged prostate presses against the urethra, causing it to narrow. It is carried out under general anesthesia and involves a surgeon passing a thin metal tube with a camera on the end through the penis to the urethra. A small wire loop is then put through the tube and heat is used to remove small parts of prostate tissue. During the operation, fluid is passed through the bladder to flush away the removed tissue. Possible side effects of TURP include: problems urinating, though this usually improves over time stress incontinence, affecting around 2 percent of patients blood in urine for the first couple of weeks after the procedure urine infection slow urine flow caused by scar tissue from the operation, affecting 4 percent of patients erectile dysfunction, affecting up to 7 percent of patients Around 65 percent of men will suffer retrograde ejaculation. This means that semen is passed into the bladder during orgasm rather than being ejaculated. Men who have retrograde orgasm experience orgasm differently and may not be able to father children through sex. Banking sperm is a treatment option for this side effect. Life after surgery The outlook for men diagnosed with prostate cancer is good. According to the American Cancer Society, the 5-year relative survival rate for prostate cancer is almost 100 percent. However, many men say that being diagnosed with prostate cancer changes their life. A diagnosis and surgery can affect everyday life, work, and relationships. Managing erectile dysfunction Phosphodiesterase type 5 (PDE5) inhibitors are drugs that help men get and keep erections. The best known of these is Viagra. A range of creams, pumps, and implants may also help, and men can be offered testosterone replacement therapy. Managing urinary incontinence Absorbent pads or pants or a urinary sheath, which drains urine from the penis to a bag, can help manage symptoms of urinary incontinence. Healthcare teams also recommend pelvic floor exercises to strengthen the muscles used during urination. For more severe cases, surgical options, such as an artificial urinary sphincter or internal male sling, may be suggested. |
|
#101
|
||||
|
||||
|
Re: Sexual Health News
Hydrocelectomy: All you need to know
https://www.medicalnewstoday.com/articles/318688.php Hydrocelectomy is a kind of surgery used to remove fluid-filled sacs called hydroceles. These form in the scrotum, the muscular pouch of skin that holds and protects the testicles. A hydrocele forms when fluid from the abdomen flows into the scrotum. A hydrocele causes swelling but is usually not painful. Some people describe it as feeling a little like a water balloon. Roughly 1 out of every 10 boys is born with a hydrocele, according to the Urology Care Foundation. Studies indicate that the condition resolves itself by the time the majority of these boys are 2 years old. Contents of this article: What are hydroceles Hydrocele diagnosis Hydrocelectomy procedure Outlook Fast facts on hydroceles Here are some key points about hydroceles. More detail and supporting information is in the main article. Hydroceles can also develop in adult males, often following an injury that causes swelling A physical exam is the first step in diagnosing a hydrocele Hydrocelectomy is usually considered minor surgery and performed on an outpatient basis Without a hydrocelectomy or other forms of treatment, hydroceles may continue to swell, though most resolve on their own. In children, a hydrocele is treated mainly to prevent a hernia from developing. What are hydroceles? Communicating hydroceles In a communicating hydrocele, there is a direct path between the abdomen and the scrotum. Also, an inguinal hernia, where part of the small intestine drops into the scrotum, may be present. A communicating hydrocele may change its size during a day, growing larger as fluid drains into the scrotum from the abdomen. Non-communicating hydroceles In a non-communicating hydrocele, the fluid stays inside the sac but is not absorbed by the body. Hydrocele of the cord is a particular kind of non-communicating hydrocele, where the condition develops further up in the scrotum. This type of hydrocele may sometimes be confused with an inguinal hernia, cyst, tumor, or other problem with the groin area. Hydroceles in children For infants with congenital hydroceles, the condition develops between the 28th and 32nd weeks of pregnancy, when a muscle in the scrotum opens to let the testes drop. In some cases, the muscle stays open longer than is needed, doesn't close properly, or opens again, allowing fluid from the belly to flow into the scrotum and form a hydrocele. Premature birth, cystic fibrosis, and other conditions may increase the likelihood of problems with closure of this muscle. Hydroceles in adults In adults, hydroceles affect about 1 percent of men over 40 years. Radiation treatment for prostate cancer may increase the risk of developing a hydrocele. When non-communicating hydroceles develop in adult men, the cause is usually unknown. A hydrocele itself does not cause pain, but men may experience discomfort due to the size and weight of the swollen scrotum. Even in adults, the condition may disappear on its own in a few months, but if it does not, medical attention is needed and a person should consider having a hydrocelectomy. Hydrocele diagnosis Upon examination, a doctor will attempt to feel the condition of the testicle. Ordinarily, this is not possible, due to the surrounding sac of the hydrocele. Before performing a hydrocelectomy, a doctor may carry out a procedure called transillumination, which involves: Shining a light through the scrotum, looking for fluid, which would indicate the presence of a hydrocele. Conducting an ultrasound examination to determine whether the observed swelling is a hydrocele. Treating the hydrocele with aspiration, using a needle to drain fluid out of the scrotum. After a positive diagnosis, a doctor may recommend a hydrocelectomy. What is the procedure for hydrocelectomy? The procedure takes place under a general anesthetic. If an infant has a hydrocele that does not go away on its own, surgeons will wait until the child is at least 1 to 2 years old before operating. The steps involved with a hydrocelectomy depend on whether the hydrocele is communicating or non-communicating: Non-communicating hydrocele: Surgeons make an incision in the scrotum, remove the sac, drain the fluid, and close the incision. Communicating hydrocele: Treatment is slightly more complicated; doctors make an incision through the groin so that they can treat a hernia, if present, at the same time as removing the hydroceles. Even if there is no hernia, doctors take this approach to prevent a hernia from developing in the future. Laparoscopic hydrocelectomy Some surgeons will conduct a hydrocelectomy through laparoscopic (keyhole) surgery, inserting a tube equipped with a camera through the abdomen. In some cases, individuals and their doctors opt for draining the hydroceles, which can be effective. However, this procedure carries a greater risk of the hydroceles returning. Outlook A hydrocelectomy requires a general anesthetic, and most people go home a few hours after having the operation. So, it is important to talk to the surgeon about what to expect for themselves or a child during recovery. It is a good idea to find out what, if anything, merits a call to the doctor. For the first week or so after the procedure, most individuals will experience pain that requires medication. In addition to pain relievers, using an ice pack on the affected area can also help. Some individuals may need to use special bandages or a drainage tube during their recovery process. For a few weeks after surgery, swelling may continue. Activity should be limited, depending on the individual's age and the extent of the procedures performed. Give children sponge baths, rather than a soak in the tub, for around 10 days after a hydrocelectomy. For about 3 weeks after the procedure, children should not play with rocking horses, ride bicycles and other straddle toys, or take part in sports. |
|
#102
|
||||
|
||||
|
Re: Sexual Health News
Penile fracture: Symptoms, causes, and what to do
https://www.medicalnewstoday.com/articles/318566.php A penile fracture is a rare and alarming injury that may occur during sexual intercourse. A penile fracture is not the same as a break in a bone. Instead, it is a rupture in the two areas of the penis responsible for erections: the corpora cavernosa and the penile sheath. Because the injury can cause long-lasting damage to a man's sexual and urinary function, it is important to seek emergency medical attention. Contents of this article: What are the symptoms of a penile fracture? Causes When to see a doctor Diagnosis Treatments for a penile fracture Aftercare and recovery What are the symptoms of a penile fracture? A penile fracture is a painful injury that usually occurs in the lower two-thirds of the penis. Symptoms of a penile fracture include: bleeding from the penis experiencing dark-colored bruising to the penis having trouble urinating hearing a cracking or popping sound losing an erection suddenly pain that varies from minimal to severe According to research, penile fracture symptoms that do not include a popping sound or rapid loss of erection are usually due to another type of injury. A penile fracture will often cause the penis to take on what doctors call an "eggplant deformity," where the penis appears purple and swollen. Rarer symptoms of a penile fracture include swelling in the scrotum and blood in the urine. Other conditions that mimic the symptoms of a penile fracture include a rupture of the veins and arteries in the penis and a ruptured suspensory ligament. A doctor can use imaging techniques and conduct a physical exam to determine the difference between the conditions. Causes The penis has an area of sponge-like tissue called the corpus cavernosa. When a man has an erection, the blood in the penis concentrates in this area. When the penis is erect, one or both sides of the corpus cavernosa can snap, resulting in a penile fracture. A penile fracture will usually only occur when a man's penis is erect. A flaccid penis does not typically fracture because the corpus cavernosa is not as enlarged as when the penis is erect. According to one review, most cases of penile fracture in the United States occur during intercourse. The injury usually happens when a man is thrusting against the pubic bone or the perineum, which can cause the corpus cavernosum to snap or break. Men are not necessarily having rough sex when a fracture occurs, but may be in a position where the penis is more likely to hit against a bone. However, a penile fracture has also been known to occur in the following circumstances: rolling over in bed onto an erect penis hitting an erect penis on something, such as a door frame or furniture falling onto an erect penis When to see a doctor If a man suspects he has a fractured penis, he must seek immediate medical attention. Doctors consider a penile fracture a urological emergency because it has the potential to affect a man's sexual and urinary function permanently. Most men will seek treatment at an emergency department. The faster a man can see a doctor and have the fracture treated, the more likely he is to experience a full recovery. Diagnosis A doctor can typically diagnose a penile fracture by asking questions about how the fracture occurred and inspecting the penis. Imaging studies, such as an X-ray, may also be used. Also, a doctor may use an ultrasound, which uses sound waves to detect abnormalities and locate the exact area or areas where the penis was damaged. If a doctor cannot identify the tear using ultrasound, they may use magnetic resonance imaging (MRI) instead. Treatments for a penile fracture Treatments for a penile fracture can include at-home care and surgical repair. At-home treatments include: Applying cloth-covered ice packs for 10 minutes at a time to reduce swelling. Using a Foley catheter to empty the bladder and reduce trauma to the penis. Taking anti-inflammatory medications, such as ibuprofen, to reduce pain and swelling. Occasionally, a doctor will also recommend wrapping the penis or wearing special "splints" to position the penis in a way that reduces pressure. Using at-home treatments alone has been shown to cause high rates of complications following a penile fracture. Examples of these include pain when getting an erection, a severe angle to the penis, and inability to achieve an erection. As a result, many doctors recommend surgical repair and treatment. According to some research, surgery results in better outcomes for people with penile fractures. Surgical treatment can vary based on the extent of a man's injuries. Examples of repairs that may be made after a penile fracture include: getting rid of a hematoma or buildup of blood due to the fracture stopping bleeding of any damaged blood vessels closing any cuts or lacerations to the penis that may be causing bleeding. If a man's urethra is also damaged, a doctor may need to repair it as well. To repair the penile fracture, a doctor will make an incision in the skin of the penis to access the one or more torn areas. The surgeon will repair these tears with stitches. If a man does not seek treatment for a penile fracture, it is possible that he could experience a permanent penile deformity. An untreated penile fracture may also lead to difficulty maintaining an erection, which is known as erectile dysfunction. Aftercare and recovery The ease of recovery following a penile fracture usually depends on the severity of the injury. While most men will be able to go home after the procedure, a doctor will usually advise them to refrain from sexual activity for at least 1 month to allow the surgical site to heal. In rare instances where a man has difficulty avoiding an erection for the duration of the recovery period, a doctor may prescribe medications to reduce the likelihood an erection, such as sedatives or hormones. Prompt treatment of a penile fracture is vital to ensure a man can return to his full sexual and urinary function. |
|
#103
|
||||
|
||||
|
Re: Sexual Health News
Sperm count more than halved in Western men
https://www.medicalnewstoday.com/articles/318588.php In the largest study of its kind, researchers find that sperm count in Western countries has more than halved in recent decades. Outside of these countries, however, the decline is not significant. The question of whether or not sperm count is declining has been hotly debated for many years within the scientific community. However, no firm conclusion has been reached. Of course, a reduced sperm count has important implications for reproduction, but this is not the only reason for alarm; low sperm count has been shown to increase the risk of all-cause mortality and morbidity. For instance, a study published in 2014 concluded that "those with abnormal semen parameters have a higher risk of death, suggesting a possible common etiology between infertility and mortality." Also, reduced sperm count is associated with deformation of the penis (hypospadias), a testicle that has not moved into the scrotum (cryptorchidism), and testicular cancer. Another general concern is that sperm count and other measures of semen quality might be a sign that we are living in a toxic environment. The more we understand about this, the better we can approach making informed changes to the chemicals that we use every day. Gathering data on sperm count With these factors in mind, a group of researchers recently set out to conduct a large-scale systematic review and meta-analysis of sperm count trends. For the study, a group from the Hebrew University-Hadassah Braun School of Public Health and Community Medicine in Israel joined forces with the Icahn School of Medicine at Mount Sinai in New York City, NY. Their results are published this week in the journal Human Reproduction Update. They screened 7,500 studies and completed a meta-regression analysis on 185 studies carried out from 1973 to 2011. The results were clear and surprising. Men from Europe, North America, Australia, and New Zealand had a 52.4 percent decline in sperm concentration and a 59.3 percent decline in total sperm count. In contrast, no significant decline was found in men from Asia, South America, and Africa - although there were fewer studies to analyze in these regions. Worryingly, the rate of decline in Western men did not appear to be slowing; "the slope was steep." Even when the analysis was limited to studies from 1996 to 2011, the trend was still significant. The implications of reduced sperm count Since 1992, the question of whether sperm count is steadily dropping has been widely debated. Although earlier studies have addressed this problem with varying results, the current research has a broader scope. To ensure the analysis was as accurate as possible, the researchers controlled for a thorough array of potential factors. These included abstinence time, method of semen collection, how the sperm were counted, age of participant, how the study population was selected, and how many samples were given per man. Quote:
Although the current study did not address the direct cause, decline in semen quality has been previously associated with pesticides, heat, lifestyle factors, diet, smoking, stress, and body mass index (BMI). The researchers ask whether the declining sperm count may be the proverbial "canary in the coal mine." Because the study analysis was so detailed, and the dataset so varied - namely, it was spread evenly across 39 years and 50 countries - the findings are particularly robust, and they are, therefore, particularly worrying. With connections already drawn between reduced sperm count and overall mortality, the authors write, "Research on causes and implications of this decline is urgently needed." |
|
#104
|
||||
|
||||
|
Re: Sexual Health News
Paraphimosis: Symptoms, treatment, and prevention
https://www.medicalnewstoday.com/articles/318833.php Paraphimosis is when the foreskin is pulled back behind the tip of the penis and becomes stuck there. The retracted foreskin and the penis become swollen, fluid can build up, and the foreskin is unable to return to its original position. Paraphimosis should not be confused with phimosis, which is when the foreskin cannot be pulled back from the tip of the penis. Typically, this occurs in younger children and is not usually a serious condition. Paraphimosis, on the other hand, is painful and a medical emergency that needs to be treated quickly. If ignored, it can affect blood flow to the tip of the penis. In rare cases, this may cause the penis tip to be damaged, or even lost. Contents of this article: How is paraphimosis caused? Symptoms How is paraphimosis treated? Prevention Diagnosis Complications Outlook Fast facts on paraphimosis: Pain, swelling, and an inability to retract the foreskin are the main symptoms. Paraphimosis can usually be resolved manually. If not, minor surgical treatment may help. Personal hygiene can go a long way towards preventing paraphimosis. If treated quickly, the condition is not serious. How is paraphimosis caused? A foreskin that is left retracted long enough for swelling to occur. This can happen during a medical examination, after cleaning, or after urination. A tight foreskin that is retracted, causing the penis to swell. This results in the foreskin not being able to move back to its natural position. Vigorous sexual activity, penile piercing, and use of a constricting penile ring to enhance erection by compression. Paraphimosis can also result from the following medical conditions or procedures: Infection, due to various factors, including poor personal hygiene. Scarring, caused by repeated infection of the foreskin, or by forced retraction of the foreskin in young boys. A circumcision that has not be done correctly. Swelling of the penis and foreskin, due to insect or spider bite. Paraphimosis in older men is often due to one of the following: Diabetes, causing chronic inflammation of the penis and foreskin. This makes paraphimosis more likely. Catheterization that is done without the foreskin being returned to its natural position. In children, the foreskin does not retract at all until about 2 years of age. Most boys will have a retractable foreskin by the age of 10, and forcibly pulling the foreskin back before it is ready to do so can cause scarring that can go on to cause paraphimosis. Symptoms Paraphimosis is characterized by the following: inability to pull the retracted foreskin back over the head of the penis swelling of the end of the penis discomfort and pain Other symptoms may include: redness, tenderness inability to urinate dark blue or black tissue on the end of the penis How is paraphimosis treated? Pressure is applied to the swollen penis for 5-30 minutes, usually with a saline swab. Ice can also be used. These treatments can compress the swelling, so it is easier to push the penis while pulling the foreskin back into place. If manual manipulation is unsuccessful, then a puncture technique may be required. This treatment usually needs some form of local anesthesia or sedation. A needle is used to puncture the foreskin in different places. This allows built-up fluid to be released and for the manual manipulation of the foreskin over the penis to become easier. More severe cases might require a small incision or slit in the foreskin to relieve restriction and to allow the swelling to subside. This procedure requires local anesthesia. In some cases, circumcision may eventually be required. Prevention After the foreskin has been retracted, it should be replaced over the head of the penis. Cleanliness helps prevent paraphimosis, as well. It is important to clean under a retractable foreskin properly. The foreskin should always be returned to its natural position after cleaning. Circumcision, when done correctly, prevents paraphimosis from occurring. Diagnosis A physical examination is enough for a doctor to confirm a diagnosis of paraphimosis. It is usually easy to see and will be characterized by a tight band of foreskin trapped behind the head of the penis. Sometimes, however, this constricting foreskin band can be completely hidden by surrounding swollen tissue. As part of a diagnosis, a person will usually be asked some question to establish background information, including any symptoms, problems, or activities relating to the penis or foreskin. Additional tests are usually not required to confirm a diagnosis. During an examination, a swab may be taken to pinpoint the type of infection that caused the paraphimosis. If there has been a circumcision, or removal of the foreskin, this will rule out a paraphimosis diagnosis. Complications Complications of paraphimosis are secondary conditions and other disorders that are caused by it. Often the difference between the symptoms and the complications of paraphimosis are not always clear. In severe cases, or if the paraphimosis is untreated, the following complications can occur: damage to the penis tip impaired or loss of blood flow gangrene loss of the penis tip Risk factors for having paraphimosis include a person's age. The condition can occur at any age but is most common in adolescence. It also occurs in older men, typically those who have diabetes, those who need catheterization, or those who have a history of bacterial infection. Outlook The outcome is likely to be excellent if the condition is diagnosed and treated quickly. A small amount of bleeding can occur, as the skin is retracted, but long-term negative outcomes are rare. Recurrence of paraphimosis can be fairly common. Circumcision can prevent a reoccurrence once the swelling has subsided. If paraphimosis is left untreated, serious damage can occur, including loss of blood flow and potential loss of the tip of the penis. |
|
#105
|
||||
|
||||
|
Re: Sexual Health News
Yellow semen: Causes of different semen colors
https://www.medicalnewstoday.com/articles/318893.php While semen is typically a whitish-gray color, there are some instances when semen may appear as a different color, which is commonly yellow. Sometimes producing an unusual colored semen is a once-only occurrence. Other times, a man may notice a more consistent change in the color of his semen. Although this occurrence is not always a cause for concern, there are some instances when semen color change can be an indicator of an underlying medical condition. Contents of this article: How are different semen colors caused? Causes of yellow semen Should I see a doctor? Treatments for yellow semen Other semen color changes Outlook Fast facts on yellow semen: Semen is a gel-like liquid that males emit during ejaculation or sexual release. Semen contains sperm, which can fertilize a female egg. Several glands and male reproductive organs are responsible for producing semen and transporting it for ejaculation. Dysfunction of one or more of these areas could lead to semen color changes. Treatments for unusual colored semen will depend upon the underlying cause. How are different semen colors caused? Semen as a substance is a combination of secretions from the male reproductive glands as well as sperm. Changes and disruption to these areas are what cause color changes. The following are responsible for semen production: Epididymis and testicles: The testicles are the organs responsible for producing sperm. The epididymis is the tube that transports sperm from the testicles to the vas deferens. Seminal vesicles: These produce a significant portion of the semen's volume. These glands produce secretions that are high in a sugar called fructose, which provides nutrients to the sperm. Prostate gland: This gland produces a chemical called prostate-specific antigen (PSA) that causes a reaction in the gel-like semen, allowing the sperm to swim away and reach an available egg more easily. Bulbourethral and urethral glands: These glands are responsible for producing secretions that make it easier for semen to travel along the reproductive tract. Each of these parts of the male reproductive organs and glands plays a role in ejaculation. Causes of yellow semen Although semen is usually a whitish-gray color, some men may have sperm that is yellow. However, if yellow semen represents a significant color change for a man, this could be cause for concern. Some potential causes associated with yellow semen include: Urine in the semen: Semen travels through the urethra, which is the same tube that urine travels through. It is possible that some yellow-tinted urine can mix with semen, which would give semen a yellow tint or cast. Jaundice: This results when the liver has difficulty breaking down bilirubin, a by-product of red blood cell destruction. Jaundice most commonly causes yellowing of the eyes but can cause the skin and the semen to appear yellow too. Abnormally high white blood cells: Inflammation can produce excess white blood cells. These can be released via the semen, a condition known as pyospermia or leukocytospermia. Additional white blood cells can cause semen to appear yellow. These can be the result of an infection. STIs: A sexually transmitted infection, such as chlamydia, herpes, or gonorrhea may cause yellow semen. In this instance, a man's semen may also have an unpleasant smell. Dietary changes: Eating foods that contain dyes can cause yellow semen. The smell of ejaculate may also change if a man eats strong-smelling foods, such as garlic, onions, asparagus, or broccoli. Infrequent ejaculation: If a man has not ejaculated in some time; the semen is more likely to have mixed with urine. Should I see a doctor? While semen that is light yellow is not usually a cause for concern, there are instances when a man should see a doctor for yellow semen, especially when the semen is a dark yellow. If a man has other symptoms, such as yellowing skin, fever, the semen smells foul, or he experiences pain when ejaculating, he should see his doctor. Treatments for yellow semen Treatment depends on the underlying cause. If an infection has caused yellow semen, a doctor may prescribe antibiotics or anti-viral medications. If a man does have yellow sperm that is consistent with a possible infection, he should refrain from sexual contact until a doctor can examine him for infections. Otherwise, he could potentially pass on an infection to his partner. A man may also try to reduce the amount of artificial dyes in his diet. Drinking more water can also help. Other semen color changes Semen can be other colors too. Some other potential color changes a man may notice include: Brown or red: Sometimes a man can experience a leak, or a blood vessel may burst around the seminal vesicles. The release of blood can cause semen to take on a brown or red appearance. If the semen continues to be red after 1 to 2 days, a man should seek medical treatment. Green-tinted: Green-tinted semen can indicate a potential infection of the prostate or surrounding tissues. A man who has green semen may need to see his doctor. If a man notices something out of the ordinary, or his semen remains discolored for an extended period, he should contact his doctor who can diagnose the potential cause and provide peace of mind. Outlook It is not completely abnormal for a man to produce semen that varies in color, texture, and even smell. The presentation can vary based on a man's diet, activities, and the amount of time since he last ejaculated. Yellow-tinted semen does not necessarily mean there is cause for concern. However, dark yellow semen that smells foul or is accompanied by other symptoms of infection or medical problems should not be ignored. |
| Advert Space Available |
 |
| Bookmarks |
|
|
 t Similar Threads
t Similar Threads
|
||||
| Thread | Thread Starter | Forum | Replies | Last Post |
| Non sexual health question | sicknasty | Sexual Health Issues | 7 | 10-01-2015 05:45 AM |
| Sexual Health Issues | Whybother | Sexual Health Issues | 2 | 24-04-2013 07:02 AM |
| DSC Sexual Health Screening | Huluman | Sexual Health Issues | 3 | 23-11-2008 08:57 PM |
| Sexual Health & Well Being | MrDevil | Sexual Health Issues | 10 | 29-03-2004 09:36 AM |
| sexual health mentor | boyrusty2000 | Sexual Health Issues | 31 | 06-08-2003 11:10 PM |