 |
|
#31
|
||||
|
||||
|
Re: Sexual Health News
Alcoholism drug could help cure HIV, study finds
http://www.medicalnewstoday.com/articles/302724.php A drug used to treat alcoholism - called disulfiram - could bring us closer to a cure for HIV, according to the results of a new study led by researchers from the University of Melbourne in Australia. Study leader Prof. Sharon Lewin, of The Peter Doherty Institute for Infection and Immunity at Melbourne, and colleagues publish their findings in The Lancet HIV. Disulfiram (brand name Antabuse) is a drug given to individuals with an alcohol use disorder to discourage them from drinking. It works by blocking an enzyme called dehydrogenase, which plays a role in metabolizing alcohol intake. Inhibiting dehydrogenase causes acute sensitivity to alcohol; if patients consume alcohol while taking disulfiram, they will experience a number of unpleasant side effects, including headache, nausea, chest pain, vomiting, weakness, blurred vision, sweating and mental confusion. But as well as helping to treat alcoholism, Prof. Lewin and colleagues found the drug could lead to a cure for one of the world's most serious and challenging diseases: HIV. Antiretroviral therapy (ART) is the primary treatment for HIV, involving a combination of at least three antiretroviral drugs that slow disease progression. While the treatment has led to reductions in HIV death rates worldwide, it is not a cure. ART is unable to eliminate HIV from patients completely; the virus can lay dormant in cells, hiding from immune system attack. But in their phase 2 clinical trial, the researchers found disulfiram helped "wake up" dormant HIV cells, allowing them to be destroyed - a "shock-and-kill" approach that researchers believe is key to curing the virus. Disulfiram 'could be the game changer we need' Numerous studies have investigated such an approach. In September, for example, Medical News Today reported on a study that suggested a class of drugs being tested for the treatment of cancer could rewaken dormant HIV cells. However, Prof. Lewin and colleagues note that to date, the drugs trialed to reawaken latent HIV have produced toxic side effects - a major barrier to moving the shock-and-kill approach forward. For their study - conducted in collaboration with researchers from the University of California-San Francisco - the team gave disulfiram to 30 HIV-positive patients in the US and Australia who were receiving ART. Disulfiram was administered daily for 3 days. Patients received 500 mg of the drug on the first day, 1,000 mg on the second day and 2,000 mg on the third day. The researchers found that the 2,000 mg dose activated dormant HIV in patients' cells without producing any toxic side effects. "The dosage of disulfiram we used provided more of a 'tickle' than a 'kick' to the virus, but this could be enough," says Prof. Lewin. "Even though the drug was only given for 3 days, we saw a clear increase in virus in plasma, which was very encouraging." Prof. Lewin adds: Quote:
"This is a very important step as we have demonstrated we can wake up the sleeping virus with a safe medicine that is easily taken orally once a day," he adds. "Now we need to work out how to get rid of the infected cell. A kick-start to the immune system might help. We have an enormous amount still to learn about how to ultimately eradicate this very smart virus." |
|
#32
|
||||
|
||||
|
Re: Sexual Health News
Pesticide exposure during teens linked to later-life sperm abnormalities
http://www.medicalnewstoday.com/articles/302012.php Men exposed to pesticides known as organochlorines during adolescence may be at higher risk for abnormal sperm, according to new research. Lead author Melissa Perry - professor and chair of the Department of Environmental and Occupational Health at the Milken Institute School of Public Health at George Washington University in Washington, DC - and colleagues publish their findings in the journal Environmental Health Perspectives. In the US, organochlorine pesticides - such as dichloro-diphenyl-trichloroethane (DDT) and polychlorinated biphenyls (PCBs) - were widely used in agriculture and insect control between the 1950s and 1970s. By the late 1970s, however, such compounds were banned in the US due to overwhelming evidence of the harm they may pose to the environment and animal and human health; they have been associated with increased risk for cancer, developmental delays and endocrine disruption. Despite these risks, some tropical countries continue to use organochlorines, and even in countries that have banned their use, the chemicals can persist in soil and water for many years. In the US, individuals may be exposed to organochlorines through high consumption of meat, dairy products and fatty fish. For their study, Perry and colleagues set out to determine how, for the first time, exposure to organochlorines during adolescence may impact sperm quality. Higher rates of sperm disomy with higher organochlorine exposure The team assessed the blood and sperm samples of 90 men aged 22-44 who lived in The Faroe Islands, where exposure to organochlorines is higher than normal due to high consumption of fish, including pilot whale meat and blubber. For 33 of the men, blood samples were also taken at the age of 14, allowing researchers to measure levels of organochlorines and determine their exposure to the pollutants during adolescence, as well as in adulthood. The researchers used an imaging technique created in Perry's lab to assess the men's sperm samples for signs of sperm disomy, where the sperm cells possess an abnormal number of chromosomes - a condition that has been associated with infertility. The team found that the men whose blood samples contained higher levels of DDT and PCBs both in adolescence and adulthood had higher rates of sperm disomy than men whose blood samples contained lower levels of the pesticides. The researchers say their findings support those of a previous study they conducted, which found American men who were part of a couple being treated for infertility and who had higher organochlorine concentrations in their blood were more likely to have sperm disomy. Pesticide exposure 'may cause reproductive problems years later' According to the investigators, their findings should prompt policymakers to enforce harsher regulations for the use of pesticides and other chemicals that may pose harm to public health. "This study, and others like it, suggest that any decisions about putting biologically active chemicals into the environment must be made very carefully as there can be unanticipated consequences down the road," says Perry. In addition, the team believes their findings emphasize the need for further investigation into how pesticide exposure may affect a man's sperm quality. Perry adds: Quote:
The Washington Toxins Coalition recommend checking with state advisories before consuming sport-caught fish or shellfish, as they can be high in DDT and PCBs. Atlantic salmon, wild striped bass, blue crab and American eel are some of the commercial fish that contain higher pesticide levels. |
|
#33
|
||||
|
||||
|
Re: Sexual Health News
Never knew that actually, thanks for sharing it
|
|
#34
|
||||
|
||||
|
Re: Sexual Health News
abit more info on the chickenpox virus
once u get chickenpox...u are sort of immune to the virus...however the virus could lie in your nerves... the next time the virus reactivate and attack you...you get shingles(herpes zoster) instead of chickenpox. shingles isnt as contagious as chicken pox and it isnt passed from person to another... but note that the virus can be pass on to someone who has never had chicken pox...e.g if u have not had chicken pox and come in contact with someone with shingles then u could get chicken pox. |
|
#35
|
||||
|
||||
|
Re: Sexual Health News
A window into sexuality
http://www.medicalnewstoday.com/releases/303528.php New research from of the Sexuality and Gender Laboratory at Queen's University shows that heterosexual women have more diverse patterns of sexual response than previously reported. Research on women's sexual orientation and patterns of sexual response has previously focused on women's genital and subjective sexual arousal relative to their sexual identity, as heterosexual, bisexual or lesbian. Among women, however, there is significant diversity among women in their sexual attractions to other women and men, regardless of sexual identity. For example, a substantial minority of heterosexual women (20 per cent in some studies) also report some attraction to women. In the first study, women watched short videos, and in the second study, women listened to stories about interacting sexually with a woman or a man. Genital response was measured with a vaginal photoplethysmograph (a clear acrylic device that illuminates the capillary bed of the vaginal wall) and participants also self-reported their sexual arousal. In both studies, Meredith Chivers (Psychology) showed that only heterosexual women who were exclusively attracted to men showed similar genital responses to both female and male sexual stimuli. Heterosexual women who also report some attraction to women, however, showed a different pattern of response; their genital responses were greater to female stimuli, similar to other sexually-diverse women. "Both exclusively and predominantly androphilic women (women attracted to men) showed sexual response patterns that differed from their self-reported sexual attractions. Sexually-diverse women showed genital and self-reported arousal responses that were more similar to their self-reported sexual attractions," says Dr. Chivers. "As a whole, this research illustrates the complex relationship between sexual identity, sexual attraction, sexual arousal and genital responses to sexual stimuli." Recently, research has misinterpreted this current study to suggest that heterosexuality doesn't exist in women because heterosexual women show sexual responses to female stimuli. The current study highlights how this interpretation is incorrect; women's sexual identity, attractions and patterns of sexual response are not interchangeable, such that a woman's sexual desires and attractions cannot be deduced from her sexual response patterns. "Instead, this research provides a window of opportunity to understand how women's sexual response relates to her experience of sexual attraction and desire, addressing gaps in contemporary models of sexual response," says Dr. Chivers. Based on the findings that self-identified heterosexual women respond to both female and male sexual stimuli, researchers could next explore how exposure to mainstream sexual media, in which women are routinely objectified, and where sexual interactions between two women are becoming commonplace, affects patterns of sexual response. The results of the research were published in PLOS ONE. |
|
#36
|
|||
|
|||
|
Re: Sexual Health News
Thanks man.
This is better than some Medical Education talks I attend! Much more informative. |
|
#37
|
||||
|
||||
|
Re: Sexual Health News
Quote:

__________________
Tips for ALL samsters.
|
|
#38
|
||||
|
||||
|
Re: Sexual Health News
Shared genetics in humans and roundworms shed light on infertility, Rutgers study finds
http://www.medicalnewstoday.com/releases/303607.php Discovery could lead to more effective treatments and better contraceptives. A discovery by Rutgers scientists links a protein in sperm to the same molecule needed for reproduction in tiny roundworms and provides clues to human infertility. In a study published in Current Biology, Andrew Singson, a professor in the Department of Genetics in the School of Arts and Sciences, and colleagues from the National Institutes of Health and the College of William and Mary in Virginia, identified a protein, SPE-45, on the sperm of C. elegan worms that help bind sperm to eggs during fertilization. It is the same as the Izumo protein considered essential for humans and other mammals to reproduce that was discovered a decade ago by Japanese scientists who named it after a marriage shrine in Japan. "Humans and worms are connected by a common ancestor that lived more than 700 million years ago and this discovery will give us insight into their shared genetics and fertility pathways," said Singson, a principal investigator at the Waksman Institute of Microbiology. The research suggests that a common ancestor to both worms and humans had a SPE-45/Izumo-like gene that was required for sperm to function properly at fertilization, said Singson, who has been researching the biological process of fertility for the past two decades. "Twenty years ago when we started this research, we predicted that we would find the genes that are required for fertility from worms to humans," said Singson. "Now we know that this kind of molecule functions the same way beyond the mammalian branch of the tree of life." In the United States, one in eight couples has fertility problems. While about 70 percent of the cases can be attributed equally to the man or woman, 30 percent of the time no explanation can be found. In the new Rutgers study, scientists found that worms produced normal-looking sperm but could not create offspring because the sperm cell lacked the SPE-45 protein on its surface similar to sperm in humans and other mammals that lacked the Izumo protein. Blocking the protein prevents sperm from binding and fusing with the egg. "The protein works like molecular Velcro and helps the sperm and egg bind and fuse," said Singson. "This type of finding can play an indispensable role in understanding the biological process." The discovery was corroborated by a team of scientists working at Emory University in Georgia and Setsunan University in Japan. Taking a different approach and using computer analysis to look at DNA sequences, this international team came up with the same conclusion which was also published in Current Biology. Comparing the worm and mammalian DNA sequences they created a hybrid SPE-45/Izumo molecule that can cure infertility in worms. "This makes the results much more solid because two research groups have basically validated the results of the other," Signson said. Since studying human infertility directly is very challenging due to many ethical and experimental limitations, making a genetic connection between worms and humans will help in future treatments because scientists can do experiments in worms to learn more about the function of Izumo-like molecules that they cannot do in mammals, Singson said. "Finding new fertility genes in the worm can help us further understand the molecular basis of human fertility," he said. "The end result of this knowledge could be more informed and effective treatments for human infertility and reliable contraceptives for both sexes." thanks doc  |
|
#39
|
||||
|
||||
|
Re: Sexual Health News
Scientists draw evidence-based blueprint for HIV treatment, prevention
http://www.sciencedaily.com/releases...1201114753.htm For many years, clinicians debated the best time to start antiretroviral therapy (ART) for HIV infection, with some worrying that the risks of treatment in terms of drug toxicities could outweigh the benefits of controlling the virus. In a new commentary, scientists from the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health, argue that the results of three large clinical trials definitively prove that the benefits of starting ART early in infection outweigh any theoretical risk. Together, the findings from the NIH-funded SMART study reported in 2006, HPTN 052 study in 2011 and START study this year conclusively demonstrate that starting ART promptly after HIV diagnosis protects the health of the infected individual while preventing HIV transmission to uninfected sexual partners, the authors write. NIAID Director Anthony S. Fauci, M.D., and colleague Hilary D. Marston, M.D., M.P.H., also note that the results of the IPERGAY study, published concurrently with their commentary online by the New England Journal of Medicine, represent important new data on HIV prevention. The study, conducted in France and Canada, focused on the use of ART for HIV prevention, a practice known as pre-exposure prophylaxis (PrEP). The IPERGAY researchers found that men who have sex with men and transgender women at high risk for HIV infection who took PrEP around the time of sexual activity were 86 percent less likely to acquire HIV than similar individuals who took a placebo. According to Drs. Fauci and Marston, this finding is further evidence of the power of PrEP to prevent HIV infection in high-risk populations. The combination of PrEP and prompt initiation of ART for infected individuals offers a promising blueprint to bring about an end to the HIV/AIDS pandemic, the authors write. Now, the scientists conclude, realizing the promise of early ART and PrEP depends on whether sufficient global political will can be mustered to provide sufficient human and financial resources to scale up HIV testing and treatment throughout the world. |
|
#40
|
||||
|
||||
|
Re: Sexual Health News
"male circumcision reduces the risk of heterosexually acquired HIV infection in men by approximately 60%"
http://www.who.int/hiv/topics/malecircumcision/en/ There is compelling evidence that male circumcision reduces the risk of heterosexually acquired HIV infection in men by approximately 60%. Three randomized controlled trials have shown that male circumcision provided by well trained health professionals in properly equipped settings is safe. WHO/UNAIDS recommendations emphasize that male circumcision should be considered an efficacious intervention for HIV prevention in countries and regions with heterosexual epidemics, high HIV and low male circumcision prevalence. Male circumcision provides only partial protection, and therefore should be only one element of a comprehensive HIV prevention package which includes: the provision of HIV testing and counseling services; treatment for sexually transmitted infections; the promotion of safer sex practices; the provision of male and female condoms and promotion of their correct and consistent use. 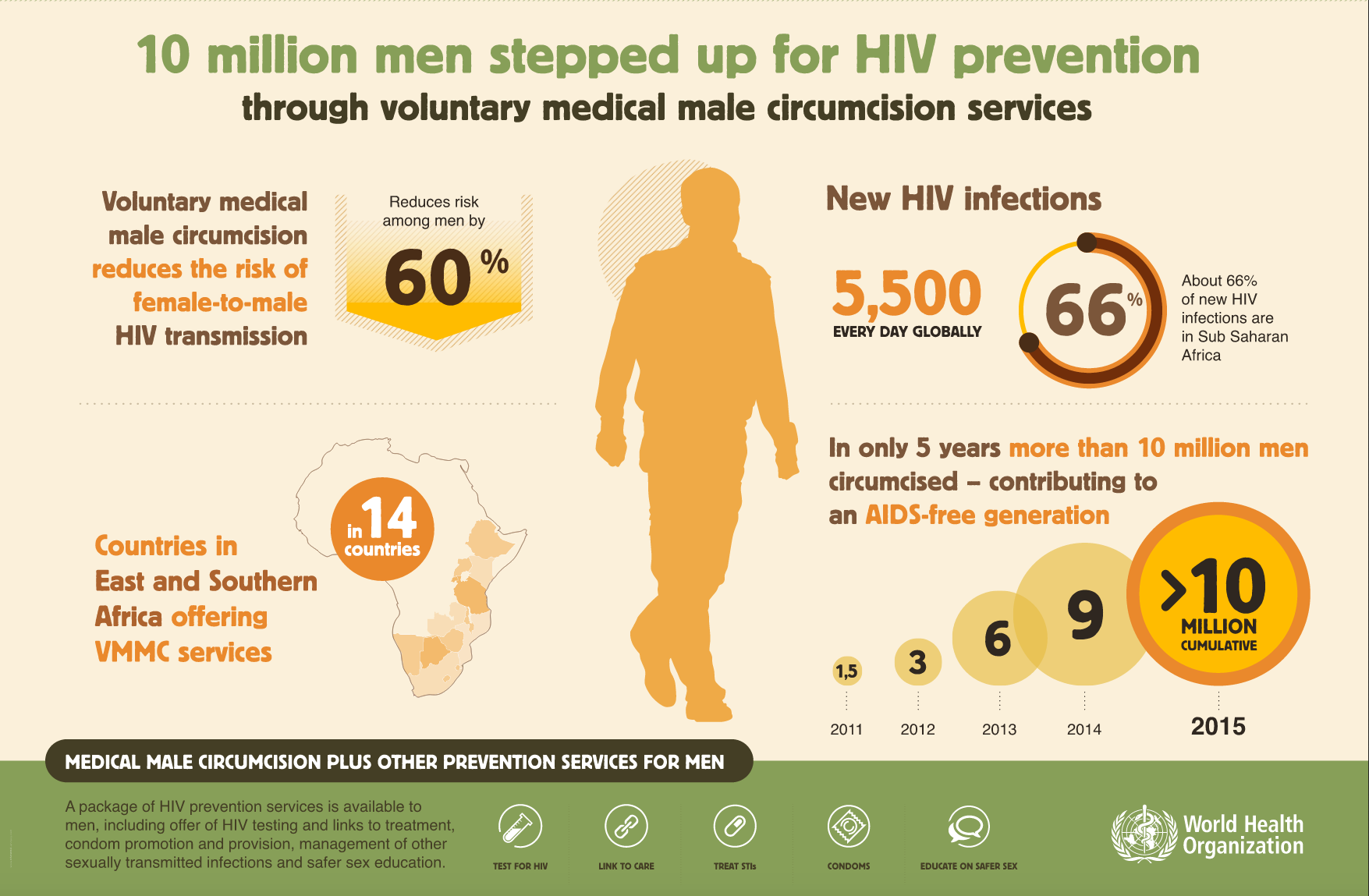 photo source from http://www.who.int/hiv/pub/malecircu...aphic_2015.pdf |
|
#41
|
|||
|
|||
|
Re: Sexual Health News
Quote:
researchers believe that the virus is triggered as the immune system weakens with age or in conditions of stress. |
|
#42
|
||||
|
||||
|
Re: Sexual Health News
The hunt for the perfect condom continues
http://www.medicalnewstoday.com/articles/303357.php Condoms prevent the spread of disease and, of course, unwanted pregnancy. Globally, more than 5 billion are sold each year, but is there still room for improvement? Since 1988, the 1st of December has been dedicated to raising awareness, fighting stigma and commemorating those lost to the disease. World AIDS Day was the first global health day, and each year since 1995, the president of the United States has made an official proclamation. By the end of 2012, there were 3.5 million people living with HIV globally and an estimated 2.3 million new HIV infections. Sub-Saharan Africa is the worst hit by the epidemic. In some countries, 20% of the population are infected. However, nowadays, Central Asia and Eastern Europe are experiencing the fastest spread of the disease. On a positive note, since 2001, new infections have fallen by 33% and the number of children newly infected by HIV has dropped by 52%. The battle is clearly not over. Science is dedicated to discovering better treatment, more effective prevention and, eventually, the cure for this most pervasive and destructive disease. Mahua Choudhury, PhD, assistant professor at the Texas A&M Health Science Center Irma Lerma Rangel College of Pharmacy, is part of this push. The future of condoms Chowdhury has come up with an ingenious and revolutionary design for a new condom. Rather than latex, which many people are either allergic to or simply dislike, she plans to use a hydrogel infused with plant-based antioxidants. The hydrogel in question is a strong, elastic polymer that consists predominantly of water. It is already used in contact lenses, so the challenge of safety testing is at least partially removed. What makes this condom particularly special is the addition of a plant-based antioxidant. This compound has been found to have anti-AIDS properties. If this innovative condom breaks, the antioxidant is released and prevents the virus from replicating. But the innovation does not end there. These particular antioxidants - flavonoids - are also predicted to heighten sexual enjoyment. What is a flavonoid antioxidant? Flavonoid antioxidants are found in many fruits, vegetables, leaves and grains. Some types of flavonoids, like quercetin, are already available in supplement form. These flavonoid antioxidants can enhance feelings of pleasure by promoting the relaxation of smooth muscle and raising arterial blood flow. Thirdly, flavonoids help keep nitric oxide levels elevated, which work to stimulate and maintain erection. Chowdhury's mission was to create a condom that would not only be an effective AIDS barrier, but also something that people would actually want to use. She says: Quote:
The competition this year was focused on finding an extremely low-cost, latex-free condom. Choudhury was one of 54 applicants selected out of 1,700 to receive the funding. The condom is not yet ready for market - extra testing is needed - but the product is well underway. "We are trying to find how fast the enmeshed antioxidant can release, and we don't know if it will automatically release, or if you have to apply pressure," Chowdhury says. Over the next 6 months or so, the final testing will have been completed. The potential benefits of a condom that people actively want to wear and that protects against AIDS with a double-edged attack are obvious. |
|
#43
|
||||
|
||||
|
Re: Sexual Health News
Men with HIV engaging in risky sexual behavior
http://www.medicalnewstoday.com/articles/303670.php Quote:
Recent data from the US Centers for Disease Control and Prevention (CDC) suggests that the HIV epidemic is growing among MSM, while remaining relatively stable in heterosexual populations. Young MSM, or YMSM, aged 13-29 years, are particularly vulnerable to HIV, accounting for more than 25% of new infections in the US, and more than 70% of all new HIV infections among youths. Black YMSM are disproportionately affected, accounting for 61% of all new HIV infections in the US in 2009. Young transgender women are also at risk, with more than 20% of new HIV cases reported in this subgroup. Methods and aims of HIV treatment HIV testing, antiretroviral treatment, adherence and viral suppression among YMSM with HIV play a key role in preventing new infections. Treatment for HIV aims to decrease the level of virus in the blood to an undetectable viral load. If a person has a detectable viral load, this means the amount of virus in the blood is high enough to be reliably detected; a cut-off point is fixed, below which the virus is said to be undetectable. It is thought that behavioral approaches, together with interventions to reduce risky sexual behaviors, could help improve rates of engagement in care and adherence to medication. Risky sexual behavior includes condomless anal intercourse (CAI). Patrick A. Wilson, PhD, of the Columbia University Mailman School of Public Health in New York, and coauthors examined differences in demographic and psychosocial factors between YMSM with and without a detectable viral load for HIV. The team also looked at psychosocial factors associated with CAI and CAI among YMSM with detectable viral load. The authors studied 991 YMSM with a detectable viral load, aged 15-26, at 20 adolescent HIV clinics in the US from 2009-12. Higher CAI activity among those with detectable HIV Among these participants, 69.4% had a detectable HIV viral load; 46.2% reported CAI in the past 3 months, and 31.3% reported CAI with someone of a different HIV status. More than half (54.7%) of YMSM with detectable HIV reported CAI, compared with 44.4% of those who were virologically suppressed, or without detectable HIV. Likewise, 34.9% of YMSM with detectable HIV reported CAI with a partner who was HIV-negative, while 25% of YMSM without HIV reported CAI with a different HIV status. Analyses suggest that among YMSM with HIV, those with problematic substance use are more likely to report CAI or CAI with someone of a different HIV status. Black YMSM with HIV were less likely to report CAI or CAI with someone of a different HIV status, as were transgender participants. The authors suggest that more research is needed into these subgroups, for whom relatively high rates of infection do not appear to be matched by risky behavior. YMSM with detectable HIV who told their sex partners about their HIV status were more likely to report CAI compared with YMSM who did not tell their partner about their status. Employed YMSM with detectable HIV were less likely to report CAI with a partner without HIV than those who were unemployed. The authors conclude: Quote:
|
|
#44
|
||||
|
||||
|
Re: Sexual Health News
80 percent of cervical cancers found to be preventable with latest 9-valent HPV vaccine
http://www.sciencedaily.com/releases...0511163018.htm The new 9-valent human papillomavirus vaccine, can potentially prevent 80 percent of cervical cancers in the United States, if given to all 11- or 12-year-old children before they are exposed to the virus. In addition to protecting against 80 percent of cervical cancers, the new 9-Valent human papillomavirus vaccine, which includes seven cancer causing HPV-types -- 16,18,31,33,45,52 and 58 -- has the potential to protect against nearly 19,000 other cancers diagnosed in the United States, including anal, oropharyngeal and penile cancers. This is a 13 percent increase in protection against HPV-related cancers in comparison to the first vaccines on the market, Gardasil and Cervarix, which protected against HPV types 16 and 18. These findings come from a seven-center study published in the Journal of the National Cancer Institute. The Centers for Disease Control and Prevention initiated the research effort, in conjunction with Cedars-Sinai. "This is the first comprehensive study of its kind and shows the potential to not only reduce the global cancer burden, but also guide clinical decision-making with regard to childhood vaccinations," said Marc T. Goodman, PhD, MPH, senior author of the study and director of Cancer Prevention and Genetics at the Cedars-Sinai Samuel Oschin Comprehensive Cancer Institute. The study found the 9-Valent vaccine, under the trademark of Gardasil-9, also has the potential to protect against an additional 8 percent of oropharyngeal cancers, which include the base of the tongue and tonsils. This disease is the second-most-common HPV-associated cancer. "We found that 70 percent of patient DNA tissue samples with cancer of the oropharynx harbored HPV," added Goodman. "This is a much higher percentage of HPV than observed in other studies, likely because of changes in sexual behaviors, such as increased oral-genital contact." The 9-Valent vaccine was also found to potentially increase protection from other HPV-related cancers including those of the vulva, from 71 to 92 percent; vagina, from 73 percent to 98 percent; the penis, 76 percent to 90 percent; and the anus, 87 percent to 96 percent. To compile these data, researchers examined 2,670 HPV DNA tissue samples from seven population-based cancer registries. Study authors intend to perform additional research in the future to follow up on their estimate of how well the current vaccines protect against HPV-associated cancers. |
|
#45
|
||||
|
||||
|
Re: Sexual Health News
Age of first sexual intercourse may impact teens' risk of acquiring sexually transmitted infections
http://www.medicalnewstoday.com/releases/304398.php A new study shows that earlier initiation of sexual intercourse increases the odds of experiencing sexually transmitted infections (STIs). Also, if the age at the time of first sexual intercourse is during or near to an adolescent's sexual maturation period, the likelihood of experiencing STIs increases. The findings, which are published in The Journal of Sexual Medicine, suggest that it is important to consider the time period of first sexual intercourse when considering STI risk. The results will also be a useful reference for further studies of adolescents' health and behavior. Studies Keywords: Sexually Transmitted Infection;Sexual Health;Timing;Adolescent Abstract Introduction Sexually transmitted infections (STIs) are major causes of medical and psychological problems globally, while adolescents in South Korea have recently shown rapid changes in sexual behaviors. Aims We aimed to examine the association between the age of first sexual intercourse and the experience of STIs among adolescents. Additionally, in which specific time period would more likely to get infected from sexual intercourse. Methods We used data from the 2007–2013 Korea Youth Risk Behavior Web-based Survey. Only adolescents with sexual intercourse experience (N = 22,381) were included, and multiple logistic regression analysis was performed. Main Outcome Measures One dichotomized measure and one continuous measure were assessed: (i) STIs experience (defined as having had STIs); and (ii) association between STIs experience and absolute age gap (defined as temporal differences between secondary sexual character emergence age and first sexual intercourse age). Results Approximately 7.4% of boys and 7.5% of girls reported had STI. For both boys and girls, the chance of experiencing STIs increased as the age of first sexual intercourse decreased (boys: before elementary school [age 7 or under]: odds ratio [OR] = 10.81, first grade [age 7 or 8]: OR = 4.44, second grade [age 8 or 9]: OR = 8.90, fourth grade [age 10 or 11]: OR = 7.20, ninth grade [age 15 or 16]: OR = 2.31; girls: before elementary school: OR = 18.09, first grade: OR = 7.26, second grade: OR = 7.12, fourth grade: OR = 8.93, ninth grade: OR = 2.74). The association between the absolute age gap and STI experience was examined additionally (boys: OR = 0.93, girls: OR = 0.87). Conclusions This study shows that earlier initiation of sexual intercourse increases the odds of experiencing STIs. Also as the age gap gets shorter, the odds of experiencing STIs increase. Our study suggests that it is important to consider the time period of first sexual intercourse and to reinforce a monitoring system along with the development of other preventive strategies. Lee SY, Lee HJ, Kim TK, Lee SG, and Park EC. Sexually transmitted infections and first sexual intercourse age in adolescents: the nationwide retrospective cross-sectional study. J Sex Med 2015;12:2313–2323. |
| Advert Space Available |
 |
| Bookmarks |
|
|
 t Similar Threads
t Similar Threads
|
||||
| Thread | Thread Starter | Forum | Replies | Last Post |
| Non sexual health question | sicknasty | Sexual Health Issues | 7 | 10-01-2015 05:45 AM |
| Sexual Health Issues | Whybother | Sexual Health Issues | 2 | 24-04-2013 07:02 AM |
| DSC Sexual Health Screening | Huluman | Sexual Health Issues | 3 | 23-11-2008 08:57 PM |
| Sexual Health & Well Being | MrDevil | Sexual Health Issues | 10 | 29-03-2004 09:36 AM |
| sexual health mentor | boyrusty2000 | Sexual Health Issues | 31 | 06-08-2003 11:10 PM |